
Johns Hopkins UniversityEst. 1876
America’s First Research University
Dissecting Artificial Hearts with Shelley McKellar

Can a mechanical heart replace the human heart? Technically, yes.
Today, artificial hearts are a clinical reality in the form of total artificial hearts and ventricular assist devices (or partial artificial hearts). These are life-sustaining devices that do a remarkable thing: they alter the usual course of events that when a person’s heart failed, that person died.
In doing research for my book, Artificial Hearts: The Allure and Ambivalence of a Controversial Medical Technology, I discovered a range of patient experiences with these devices. Some individuals lived months with an artificial heart, resumed many of their daily activities and underwent successful heart transplants. Others never left hospital, dying from device or disease complications.
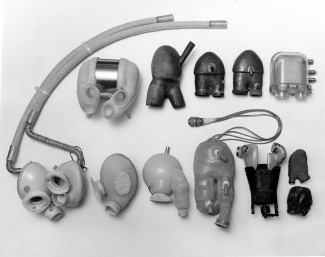
Artificial heart devices work to increase blood flow and to sustain life for end-stage heart failure patients. These devices may completely replace or assist the diseased native heart. They may be implanted or reside outside the body, for temporary or permanent mechanical circulatory support. Different heart failure patients require different cardiac devices, depending on their needs.
Artificial hearts fit well with popular imaginings of rebuilt bodies. Since the 1960s, the media tantalized the public about the possibility of replacement technology, ranging from artificial kidneys to Dacron arteries to electronic bladder stimulators, and more. Why not artificial hearts too? Who would not want a life-saving, off-the-shelf device fix for a loved one dying of heart failure?
But the history of artificial hearts is fraught with controversy, and its clinical realization was never certain. The technological complexity of building viable artificial hearts was daunting. A small but innovative group of researchers experimented with device mechanics, biomaterials, implant tolerance in the body, and other issues. They battled persistent technical problems such as blood clotting in the device, power source issues, pump malfunctions, and more.
There were horrendous first cases in which this experimental technology failed miserably. In one case, an artificial heart was implanted in a patient’s chest too small to allow surgeons to close. In other cases, patients battled infections, bleeding, strokes and device malfunction after their implants.
Poor clinical results were not hidden. Artificial heart research teams published their device challenges and setbacks in the medical literature. Journalists reported on various experimental devices that had been implanted in patients, often including color photographs from the operating room.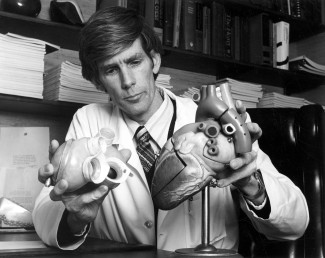
Nonetheless, NIH continued to support multiple device approaches, bolstered by the confidence and optimism of researchers that a viable mechanical heart would be forthcoming. Research and development edged forward, shifted sideways, and even abandoned problematic lines of investigation. After a decade of research, funding to develop nuclear-powered artificial hearts was halted.
How and why did this problematic technology continue to be developed for so long?
I argue that desirability rather than the feasibility or practicality of artificial hearts drove the development of this technology. Variable characterizations of success sustained the hope that viable devices would be developed, despite discouraging patient results. It was an imperfect technology, but one that became ‘good enough’ in a medical culture shaped by aggressive surgical fixes and a reluctance to accept limits.
Next year – 2019 – marks the 50th anniversary of the first total artificial heart implant. It presents an opportunity to acknowledge the remarkable technological achievement of artificial heart devices as well as to address broader health care issues of the feasibility and sustainability of end-stage disease therapies.
Shelley McKellar is the Jason A. Hannah Professor in the History of Medicine at the University of Western Ontario. She is the author of Surgical Limits: The Life of Gordon Murray and the co-author of Medicine and Technology in Canada, 1900-1950. She is also the author of Artificial Hearts: The Allure and Ambivalence of a Controversial Medical Technology.